Cognitive Behavioural Therapy vs. Medication: Which Is Right for You?
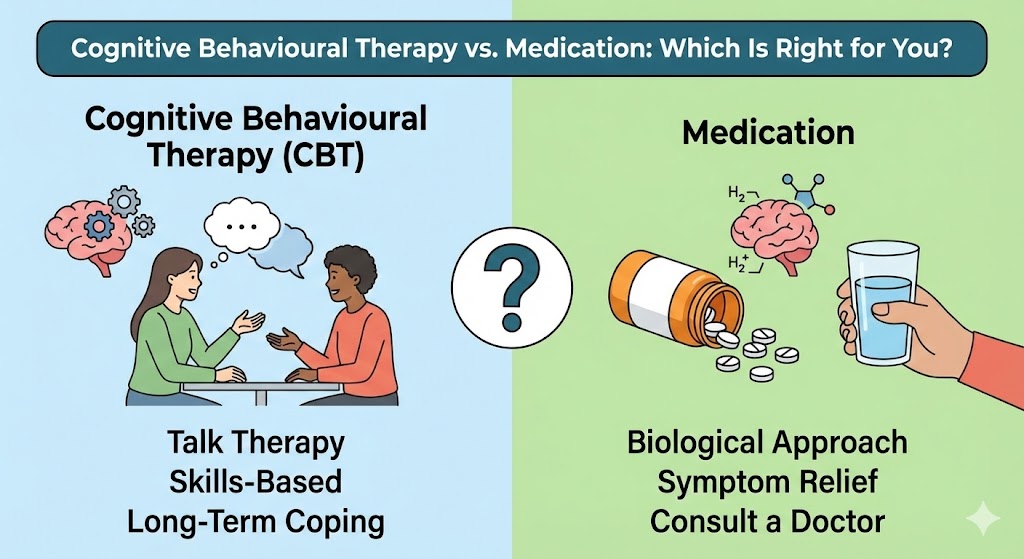
When struggling with anxiety, depression, or trauma-related symptoms, one of the biggest questions many people face is: Should I try therapy, medication, or both? At Mindfix, we understand that deciding on a mental health treatment path can feel overwhelming—especially when you’re in the midst of emotional distress.
In this blog, we’ll explore the pros and cons of Cognitive Behavioral Therapy (CBT) versus medication, how they work, and how to determine which option—or combination—may be best for your healing journey.
What Is Cognitive Behavioral Therapy (CBT)?
Cognitive Behavioral Therapy is a structured, evidence-based form of psychotherapy that helps you identify and change negative thought patterns and behaviors. It focuses on the present and provides you with practical tools to manage your emotions, reactions, and mindset.
CBT is a cornerstone of our approach to treating anxiety, depression, trauma, and more.
What Role Does Medication Play?
Psychiatric medications are often prescribed to stabilize mood, reduce anxiety, or manage symptoms of serious mental health conditions. They can help:
- Correct chemical imbalances in the brain
- Alleviate severe or persistent symptoms
- Create a more stable baseline for therapy
Common medications include:
- SSRIs/SNRIs (e.g., Prozac, Zoloft, Effexor) for anxiety and depression
- Mood stabilizers for bipolar disorder
- Antipsychotics for severe mood or thought disorders
- Anti-anxiety medications (e.g., benzodiazepines) for short-term relief
How Each Approach Impacts the Brain
Medication:
Psychiatric medications—especially antidepressants and anti-anxiety meds—work by altering the balance of neurotransmitters in your brain. For example:
- SSRIs increase serotonin, which helps regulate mood and anxiety.
- SNRIs boost both serotonin and norepinephrine to improve energy and emotional resilience.
This biological support can stabilize symptoms, especially during acute phases of depression or anxiety.
CBT:
While CBT doesn’t involve chemicals, research shows it physically reshapes the brain over time. Studies using neuroimaging reveal:
- Decreased activity in the amygdala (fear center)
- Strengthened connections in the prefrontal cortex (logic and decision-making)
- Better regulation in the default mode network (self-reflection)
This rewiring helps patients respond rather than react, making CBT a long-term tool for emotional control.
Can You Switch From Medication to CBT—or Vice Versa?
Absolutely. Mental health recovery is not a straight line, and treatment plans evolve.
You might shift from medication to CBT if:
- You’ve achieved symptom stability and want to taper off meds
- You’re interested in building coping skills for long-term management
- Side effects are interfering with your quality of life
You might start with CBT and add medication if:
- Symptoms aren’t improving fast enough or are worsening
- You experience barriers to engaging fully in therapy (e.g., panic attacks, severe fatigue)
- You need additional support to manage work, family, or school demands
Our care teams in the Partial Hospitalization Program, Intensive Outpatient Program, and Outpatient Treatment Program in Massachusetts help you navigate these transitions safely and collaboratively.
- CBT offers results without medication-related side effects.
- CBT requires commitment and active participation.
- CBT offers results without medication-related side effects.
- Many clients benefit most from CBT + medication, especially in our structured programs.
Why the Combo Works:
- Medication can stabilize mood or reduce anxiety enough to allow meaningful participation in therapy.
- CBT provides long-term tools and prevents relapse once medication is reduced or discontinued.
- Many clients in our Anxiety Therapy Programsand Depression Therapy Programs in Massachusetts start with both—and taper medication as their CBT skills grow stronger.
What Does Research Say?
CBT is just as effective as medication for many individuals with mild to moderate depression or anxiety.
Source: American Psychological Association (APA)
For severe depression, combining CBT with antidepressants offers better outcomes than either treatment alone.
Source: National Institute of Mental Health (NIMH)
CBT reduces relapse risk by up to 50% compared to medication-only treatments.
Source: Archives of General Psychiatry
Frequently Asked Questions (FAQs)
Is CBT as effective as medication?
For many individuals with mild to moderate anxiety or depression, CBT is just as effective as medication—and may even have longer-lasting results because it teaches lifelong skills for managing thoughts and behaviours.
How long does it take for CBT to work?
Most people start seeing noticeable improvement after 6–12 sessions, though results vary depending on the individual and the severity of symptoms. Consistency and practice are key.
Can I do CBT and take medication at the same time?
Yes. In fact, combining CBT with medication is often the most effective approach for moderate to severe mental health conditions. Medication can help reduce symptoms, while CBT helps you change the thinking and behaviour patterns behind them.
Can You Combine CBT and Medication?
- In many cases, the combination of CBT and medication is the most effective approach, especially for moderate to severe conditions.
How many sessions will I need?
- If you have been diagnosed with a psychological disorder and are under medical supervision, our counsellors can work alongside The number of sessions depends on the nature of your concern, its intensity, and your personal progress. Some clients notice improvement after a few sessions, while others benefit from ongoing support. Your counsellor will help you decide what works best for you.
